Birth Is Not Broken. The System Is.
The Natural Intelligence of Birth
The female body is brilliantly designed for birth. It does not require management, protocols, or external interference to function properly. Every stage of labour and birth is guided by an innate biological intelligence, carefully orchestrated by hormonal signals, emotional responses, and instinctive movements. Oxytocin, known as the hormone of love and bonding, is naturally produced by the body to facilitate rhythmic contractions and guide the baby gently through the birth canal. Endorphins, the body’s natural pain-relieving chemicals, rise alongside oxytocin, easing discomfort and creating a trance-like state that allows mothers to cope with labour’s intensity.
However, the modern medical model disregards this powerful natural intelligence, treating childbirth as a risky, pathological event that must be managed and controlled. The moment a pregnant woman enters a hospital environment, her innate birthing instincts are overshadowed by hospital protocols, timelines, invasive checks, and clinical monitoring. Rather than trusting the wisdom of the body, the medical system imposes artificial standards and routines, treating birth as a liability rather than a natural, creative process.
Hospitals frequently use fear tactics, misinformation, and manufactured urgency to pressure women into unnecessary interventions. Birth is portrayed as unpredictable and dangerous, despite evidence consistently showing that most births unfold safely and naturally without medical intrusion. This culture of fear profits from women’s distress, ultimately making mothers feel incapable, disempowered, and dependent upon a system that prioritizes convenience, efficiency, and liability reduction over true safety and emotional well-being.
Women enter hospitals believing they are making a safe choice, but instead, they encounter an environment of tension, fear, and anxiety, all of which disrupt the finely tuned hormonal balance required for smooth labour progression. The natural intelligence of birth thrives in privacy, calm, warmth, trust, and patience, all elements that hospitals routinely fail to provide. Birth should never be controlled by arbitrary timelines or aggressive interventions. When allowed to unfold in its own way, without fear or interference, the female body demonstrates extraordinary resilience, strength, and competence, affirming that birth is not a medical event but a beautifully designed biological process.
Manufactured Risks by the Medical Cult
Ironically, many of the risks presented as justifications for medical interventions in childbirth are created or intensified by the medical establishment (cult) itself. Prenatal exposure to vaccines, frequently pushed by obstetricians and healthcare providers as a protective measure, can in reality contribute directly to pre-term births, miscarriages, and other serious pregnancy complications. Despite mounting evidence, these risks are rarely disclosed or openly discussed with mothers during pregnancy.
Additionally, the medical system consistently fails to acknowledge the critical importance of cleansing the mother’s body prior to pregnancy. Environmental toxins, synthetic chemicals, heavy metals, and other harmful substances accumulate in women’s bodies over time. Studies have revealed thousands of synthetic chemicals present in placental tissues worldwide, yet the medical industry remains largely silent on this alarming fact. Instead of advocating for proper cleansing, nutritional preparation, and informed avoidance of environmental toxins, conventional medicine continues to promote pharmaceutical interventions and procedures that increase the toxic burden and disrupt maternal and infant health.
This systemic neglect of terrain health directly contributes to pregnancy complications, impaired fetal development, and long-term health problems for babies. By overlooking the root cause of these issues, environmental and bodily toxicity, the medical cult not only fails mothers but actively increases the likelihood of medical complications during pregnancy and birth. True prenatal care should emphasize cleansing, nutritional rebuilding, avoidance of harmful chemicals, and holistic preparation rather than pharmaceutical interventions or vaccines that introduce additional chemical stress.
Stress as the First Intervention
It truly all starts with emotional stress. Pregnancy can be nerve-wracking enough on its own, even without the constant pressure of having to deflect fear-mongers, misinformation, and outright lies from medical practitioners and well-meaning but misguided family or friends. From the moment a woman enters the hospital environment, doctors and nurses begin controlling the atmosphere through continuous monitoring, repeated cervical checks, strict timelines, and frequent questions about “progress.” These procedures, while portrayed as necessary and reassuring, often provoke anxiety, uncertainty, and a sense of urgency in the mother. The expectation to meet specific dilation milestones within arbitrary timeframes intensifies stress and pressure, creating an environment that is fundamentally at odds with the natural rhythm of labour.
Every unnecessary intervention triggers the body’s stress response, elevating cortisol and adrenaline levels. These stress chemicals directly interfere with the delicate hormonal balance essential to birth, particularly blocking the production of oxytocin. Oxytocin is the central hormone driving steady, rhythmic contractions, promoting dilation of the cervix, and supporting emotional bonding and relaxation. Under stress, this natural flow of oxytocin decreases significantly, causing labour contractions to become irregular, weaker, or to stop entirely.
The birthing body requires a sense of safety, privacy, warmth, and calmness to facilitate the ideal hormonal balance. Bright clinical lighting, continuous beeping of monitoring equipment, unfamiliar staff frequently entering and exiting the room, and ongoing invasive checks sabotage this ideal birthing atmosphere. The presence of strangers, interruptions, loud noises, and harsh instructions from healthcare providers keep a mother constantly alert and on edge, further elevating stress hormones. This heightened vigilance signals the body that the environment is unsafe, inhibiting the natural progression of labour.

Research supports the observation that maternal stress significantly lengthens labour, increases pain perception, and leads to further unnecessary interventions. Studies have consistently shown that higher levels of stress hormones correlate with prolonged labour, stalled dilation, and increased use of synthetic oxytocin (Pitocin) or surgical interventions like forceps, vacuum extraction, and caesarean sections (Lederman et al., 1978; Wadhwa et al., 2011). Furthermore, stress in labour has been associated with poorer postpartum outcomes, including difficulties with breastfeeding, delayed mother-infant bonding, increased risk of postpartum mood disorders, and reduced maternal confidence.
When the medical system imposes unnecessary stress as its first intervention, it disrupts the natural, instinctive rhythm of childbirth. Birth is designed to occur most efficiently in a peaceful, familiar, and supportive environment. By removing stress, supporting emotional comfort, and respecting the mother’s autonomy, labour can progress smoothly, safely, and naturally, as it was intended.
The Harmful Practice of Stretch and Sweep
The practice known as a “stretch and sweep,” or membrane sweep, is widely presented as a simple way to gently encourage labour, but in reality, it is invasive, aggressive, and frequently counterproductive. During this procedure, a healthcare provider inserts their fingers into the cervix, forcibly separating the amniotic sac membranes from the cervical lining. This abrupt disruption of the cervix’s delicate tissues often occurs long before the body signals readiness for labour. As a result, the procedure can cause immediate physical trauma, including sharp cramping, spotting or bleeding, and painful, irregular contractions that do not effectively progress labour.
Many women report feelings of shock, anxiety, or emotional distress following a membrane sweep, particularly if they were not fully informed of the procedure’s intensity or its potential side effects. This physical and emotional distress sends confusing signals to the body, further disrupting the hormonal communication essential to a smooth labour process. Oxytocin, endorphins, and prostaglandins must rise and fall in harmony to signal labour effectively, but artificial interference through stretch and sweep often throws this delicate system into disarray.
Despite being routinely offered and sometimes pressured upon women who reach full-term, scientific evidence clearly demonstrates that membrane sweeps provide little to no meaningful improvement in overall birth outcomes. Comprehensive reviews of the available studies conclude that sweeps do not consistently reduce the need for further medical induction, nor do they reliably shorten the duration of labour (Boulvain et al., 2020). Instead, the procedure is associated with unnecessary discomfort, false or ineffective labour starts, and emotional confusion for mothers who begin to doubt their body’s natural ability to birth without intervention.
Additionally, the stretch and sweep procedure poses potential risks, including increased vulnerability to inflammation, disruption of protective cervical mucus barriers, and exposure to pathogens. These concerns, alongside the documented lack of beneficial outcomes, highlight the questionable nature of this practice. It is a stark example of medical impatience overriding biological wisdom, undermining women’s trust in their bodies, and unnecessarily pushing them toward further medical intervention.
The Myth of “Due Dates”
The entire concept of a precise “due date” is fundamentally misleading and has become a cornerstone of medical interference in childbirth. Pregnancy is naturally variable, typically lasting anywhere from 37 to 42 weeks or even longer. Yet, modern obstetrics imposes a rigid 40-week timeline, calculating a specific calendar date by which a woman “should” deliver. This artificial timeline creates unnecessary anxiety, unrealistic expectations, and a false sense of urgency, setting the stage for unnecessary interventions.
In reality, only about 4 percent of women give birth precisely on their medically assigned due dates. The remaining majority birth naturally in their own timing, often weeks before or after the predicted date. A pregnancy extending beyond 40 weeks is not inherently dangerous or abnormal; it simply reflects normal biological variation. Despite this, many healthcare providers begin pressuring mothers into inductions as soon as their estimated due date approaches, implying that the baby or mother is suddenly at risk simply by going beyond an arbitrary date.
This pressure is not evidence-based. Rather, it serves hospital policies and scheduling conveniences rather than maternal or infant safety. The intense stress of feeling “late,” combined with constant medical reminders about risks associated with going overdue, artificially raises cortisol and adrenaline, hormones that directly inhibit natural labour. Thus, the fixation on due dates often creates precisely the scenario hospitals claim they wish to avoid: stalled labour, maternal anxiety, and intervention cascades.
Rejecting the artificial concept of due dates restores confidence in the natural timing of birth. Trusting the body’s signals rather than arbitrary deadlines prevents unnecessary inductions, reduces stress, and allows labour to unfold safely and naturally when both mother and baby are truly ready.
Pitocin: Synthetic Oxytocin and the Path to Crisis
Pitocin, the synthetic form of the hormone oxytocin, is routinely used in hospital settings to artificially induce or speed up labour. Although chemically similar, synthetic oxytocin acts quite differently in the body compared to natural oxytocin. Natural oxytocin is carefully regulated by intricate feedback loops involving the mother’s nervous system, emotional state, and hormonal balance, allowing contractions to gradually intensify, ebb, and flow in a manageable rhythm. This rhythmic progression is essential for both effective dilation of the cervix and the safety of the baby as it moves through the birth canal.
Pitocin, however, bypasses these delicate autoregulation pathways. Administered through an IV drip or injection (my midwife had it pre-loaded when my placenta didn’t arrive in her strange time frame, mine NATURALLY took 45 minutes – don’t do it!), it floods the bloodstream with a continuous, uncontrolled level of synthetic oxytocin, causing abrupt, intense contractions that the body cannot modulate or soften. Without the body’s natural ability to produce balancing endorphins and adjust contractions according to the mother’s comfort level and the baby’s positioning, the contractions become forceful, painful, and erratic. Women consistently report Pitocin-induced contractions as significantly more painful and overwhelming than those experienced naturally, often driving them towards additional pain relief measures such as epidurals or narcotic drugs, further compounding risks and intervention cascades.
These artificially intense and unpredictable contractions put significant stress on the baby’s physiological stability. As contractions become overly frequent and prolonged, the baby receives less blood flow and oxygen between contractions, increasing the likelihood of heart rate fluctuations. Healthcare providers label this scenario “fetal distress,” a term often interpreted as evidence that the baby is in immediate danger. Rather than acknowledging that pitocin itself is causing these distress signals, the hospital typically responds by declaring an emergency and moving swiftly toward surgical intervention.
Thus, pitocin often becomes a direct path toward an unnecessary C-section, a procedure falsely presented as lifesaving, when in truth, the “crisis” was created entirely by the medical intervention itself. Without pitocin’s aggressive interference, most mothers would have progressed naturally, safely, and without the emotional and physical trauma associated with surgical birth. This manufactured crisis not only places immediate stress on mother and baby but also sets the stage for potential long-term physical consequences, compromised breastfeeding, disrupted bonding, and difficulties in future pregnancies.
The Long-Term Consequences of C-Sections
C-sections are frequently portrayed as a routine, straightforward alternative to natural childbirth, but in reality, they are major abdominal surgeries carrying significant physical, emotional, and long-term health impacts for both mother and baby. I witnessed one in India. It was the most violent and horrific experience that deeply impacted and scarred me for life. The baby was weighed and wrapped, and put in a metal tin in the hallway. Who first bonded with this baby? Me! Insanity.
The procedure involves deep incisions through multiple layers of skin, muscle, connective tissue, and the uterus itself, resulting in internal and external scar tissue formation. These scars can create lasting problems such as chronic pelvic or abdominal pain, adhesions between organs and tissues, decreased flexibility, and ongoing stiffness. Many women experience difficulty returning to normal activities or movement patterns months or even years after the procedure due to lingering pain, weakness, or limited mobility around the incision site.
Nerve damage resulting from the surgical incision can cause long-term numbness, tingling, or hypersensitivity in the surrounding tissues, disrupting a woman’s daily comfort and bodily autonomy. Chronic inflammation following surgery is also common, leaving women more vulnerable to autoimmune responses, digestive disturbances, hormonal imbalances, and prolonged fatigue. Research has documented these complications extensively, highlighting the severity and frequency of these long-term effects (Keag, 2018).
For babies, the implications of C-section birth are equally profound. In a natural vaginal birth, babies pass through the mother’s birth canal, receiving crucial exposure to the mother’s beneficial vaginal microbiome. This microbiome exposure is essential for establishing robust digestive and cleansing processes, balanced resilience, and optimal terrain health. Babies born via C-section miss this important transfer of maternal bacteria, starting life instead with significantly altered microbiomes. Studies have demonstrated that babies born surgically exhibit reduced gut microbial diversity and are more prone to chronic disease, inflammation-related conditions, digestive issues, ADD, autism, and more from early childhood onward (Dominguez-Bello et al., 2010).
Additionally, C-sections disrupt the immediate postpartum bonding process. Unlike natural birth, surgical birth routinely interferes with immediate skin-to-skin contact, initiation of breastfeeding, and eye contact, as babies are usually born awake and ready to connect before they sleep for a long nap. Newborns are frequently separated from their mothers for medical checks and monitoring, depriving both mother and baby of critical early bonding moments. The loss of these early interactions can hinder breastfeeding success, reduce maternal oxytocin production necessary for postpartum emotional stability, and delay emotional attachment.
These long-term physical, emotional, and developmental consequences highlight the serious nature of C-sections and underscore why they should never be considered routine or harmless. Whenever possible, prioritizing natural birth processes protects the lifelong health and well-being of both mother and child.
The VBAC Myth and Medical Fearmongering
The medical industry perpetuates significant fear around vaginal birth after cesarean (VBAC), routinely steering women away from attempting natural births following prior surgical deliveries. Women who have undergone even a single C-section are often told by healthcare providers that their future options for birthing naturally have been compromised, emphasizing the risk of uterine rupture. This rare complication, frequently exaggerated by the medical community, is used to justify denying women the opportunity to birth vaginally again. However, extensive research demonstrates that the absolute risk of uterine rupture during VBAC is very low, typically below one percent (Guise et al., 2010). Despite clear scientific evidence, hospitals and medical providers persist in amplifying this rare risk to maintain control and uphold surgical birth as the default choice.
VBAC, when adequately supported and undisturbed, is not only safe but also highly successful. Studies confirm that most women who attempt VBAC achieve it without complication, especially when allowed to labor naturally, without the artificial induction methods or strict timelines imposed by hospitals. Despite these positive outcomes, medical professionals continue to pressure women toward repeat C-sections, falsely framing surgery as the responsible, safer, and more reliable option. This fearmongering is rooted in liability concerns, hospital policy convenience, and profit motives rather than genuine safety or well-being.

Women who express interest in VBAC frequently encounter systematic resistance, emotional manipulation, and outright misinformation from medical providers. Hospitals commonly present restrictive VBAC “guidelines,” such as mandatory continuous fetal monitoring, immediate IV access, or imposed time limits on labor progress, all of which actively sabotage the natural progression of birth and significantly increase the likelihood of unnecessary interventions or repeat surgeries.
The medical industry’s approach undermines women’s trust in their bodies, promoting a narrative of physical deficiency rather than recognizing the profound resilience and adaptability of the female reproductive system. The truth is that uterine tissue, like all bodily tissue, is designed to heal, strengthen, and adapt. Previous surgical birth does not automatically impair the uterus’s ability to labor safely and efficiently in subsequent pregnancies. What truly interferes with VBAC success is not the body itself, but the medical system’s fear-based control tactics and procedural interference.
In reality, many women report VBAC experiences that are not only successful but notably smoother, gentler, and less complicated than their previous surgical births. When surrounded by supportive care providers who encourage patience, trust, emotional safety, and calm, these women discover that their bodies are fully capable of birthing naturally. VBAC is more than possible—it is normal, safe, empowering, and profoundly healing.
Moreover, the process of vaginal birth involves critical physiological mechanisms that benefit the newborn’s neurological development. As the baby passes through the birth canal, gentle compression stimulates the nervous system, promoting optimal respiratory function and aiding in the clearance of amniotic fluid from the lungs (Femia, 2024). This natural compression may also play a role in reducing the risk of neurological disorders, such as attention-deficit disorder (ADD), by supporting the maturation of neural pathways during this crucial transition (JAMA Network Open, 2019). Femia Health
By embracing VBAC and trusting in the body’s innate ability to birth, women not only reclaim autonomy over their birthing experiences but also provide their babies with the neurological advantages inherent in natural delivery. This empowerment challenges the pervasive medical fearmongering and reaffirms the strength and wisdom of the female body.

The Myth of the Big Baby
Women are fully capable of safely birthing larger babies, despite medical providers frequently treating fetal size as a cause for alarm. The common narrative that having a “big baby,” medically termed macrosomia, is inherently dangerous or difficult is a fear-based myth perpetuated by the medical establishment. Obstetricians routinely warn mothers about potential complications, using ultrasounds and estimated fetal weight calculations, both of which are often inaccurate, to justify unnecessary early inductions or scheduled C-sections.
In truth, numerous studies have shown that ultrasound predictions of fetal weight can be inaccurate by as much as 15% or more. Many mothers are wrongly advised to undergo interventions or surgical births based on these misleading estimates. These interventions often lead directly to the complications they claim to prevent, such as prolonged labour, increased pain, or stalled dilation. Medical providers seldom mention that maternal positioning, mobility during labour, emotional support, and patience significantly influence the ease of birthing larger babies.
Historically and world-wide, women have routinely and successfully birthed babies weighing eight, nine, ten pounds or more without complications when supported properly and allowed to labour undisturbed. The human pelvis and birth canal are not rigid structures—they are flexible, expandable, and designed to adapt to the baby’s passage, even if the baby is larger than average. The fear of a large baby is largely a modern medical construct that dismisses the innate flexibility and adaptability of the female body.
Instead of focusing on fears about fetal size, the emphasis should be placed on nurturing the mother’s emotional comfort, encouraging her to move freely during labour, adopting optimal positions such as squatting or hands-and-knees, and trusting the natural birth process. When women labour in supportive, relaxed environments, without artificial timelines or unnecessary interventions, the birth of a larger baby can occur smoothly, safely, and naturally.
The myth of the big baby is yet another example of medicalized birth culture undermining women’s trust in their bodies and abilities. Rejecting this narrative and embracing physiological birth is vital to reclaiming autonomy, reducing unnecessary interventions, and promoting healthier outcomes for mothers and their babie
The Medicalization of Midwifery
Midwifery, once deeply rooted in intuitive knowledge, patience, and trust in natural birth, has become increasingly medicalized. Many modern midwives now function more as extensions of hospital-based obstetric practice than guardians of natural childbirth. While midwifery was historically a profession built on careful observation, emotional presence, and minimal interference, today’s midwives frequently adopt clinical protocols, time constraints, and intervention-focused practices nearly identical to hospital settings.
In recent decades, the influence of the medical system, along with strict licensing and insurance regulations, has driven midwives toward a more medically cautious approach. Many now prioritize strict timing of labour progression, recommending unnecessary procedures such as membrane sweeps or induction techniques to meet standardized labour timelines. Instead of calmly observing and gently guiding the birthing process, midwives may become anxious when labour does not align with textbook definitions of progress, pushing mothers toward premature decisions to intervene.
Fear of liability plays a significant role in this shift. Midwives operating within medicalized frameworks often feel pressured to adhere to hospital-approved policies, even if these protocols conflict with their intuition and traditional midwifery training. The pervasive threat of litigation and strict oversight has cultivated a practice style focused more on minimizing perceived risks than on genuinely supporting the physiological process of birth. This leads midwives to engage in unnecessary fetal monitoring, invasive cervical checks, early hospital transfers, or recommending interventions out of caution rather than true medical necessity.
The medicalization of midwifery erodes mothers’ trust in their bodies, reinforcing fears rather than fostering empowerment. Midwives influenced by this model frequently treat labour as something inherently risky or unpredictable, viewing deviations from strict standards as problems to be solved rather than variations of normal physiology. This mindset undermines the fundamental role of midwifery as a practice rooted in patience, trust, and reverence for the body’s wisdom.
Birth requires midwives who deeply understand and honour its natural rhythms, who observe and respond intuitively rather than impose medical guidelines. Returning to traditional midwifery practices: prioritizing emotional support, hands-off observation, and respecting natural physiological timing, is crucial. Genuine midwifery does not rely on medical backup for reassurance; it relies on the profound, ancient wisdom of women’s bodies and the timeless practice of calmly bearing witness to birth without interference.
Proof that Birth Works Naturally
The Farm midwives, led by renowned midwife Ina May Gaskin, provide powerful, undeniable proof that natural birth, free from medical interventions, is not only possible but consistently safe and successful. Operating from their community in rural Tennessee since the early 1970s, the Farm midwives carefully documented thousands of births, meticulously tracking outcomes to demonstrate the inherent safety and efficiency of physiological childbirth. Their comprehensive data, spanning decades, revealed remarkably low rates of interventions—less than one percent—far below national averages.
The success achieved at The Farm was based on straightforward principles: patience, emotional trust, proper nutrition, physical preparation, and attentive, supportive care. Women were consistently treated with deep respect and empowered to trust their bodies’ innate capacity for birth. This environment, intentionally devoid of fear-based medical narratives, allowed mothers to labour confidently, supported by midwives who viewed birth as normal, healthy, and reliable.
Birth outcomes from The Farm astonished mainstream obstetrics, demonstrating minimal complications, fewer tears or injuries, significantly reduced postpartum issues, and lower infant distress than typical hospital births. The vast majority of births proceeded smoothly, calmly, and without the stress or urgency common in hospital settings. Birth trauma and postpartum emotional distress were notably rare, highlighting the emotional safety and empowerment fostered by this non-medicalized approach.
In her influential book Ina May’s Guide to Childbirth (Gaskin, 2003), Ina May presents numerous documented birth stories that illustrate the power of the female body when supported properly. These stories challenge prevailing fears about childbirth by providing concrete evidence that natural birth is not only feasible but reliably successful. Women who previously doubted their bodies’ abilities found renewed confidence and trust when immersed in a supportive atmosphere free from unnecessary interventions.
Ina May Gaskin’s work proves conclusively that most complications associated with childbirth arise from unnecessary medical interference rather than from birth itself. The Farm midwives’ exceptional results serve as compelling evidence that when birth is respected and women are supported patiently and compassionately, interventions become rare exceptions rather than routine procedures. This extensive real-world evidence stands as a powerful testament to the wisdom, strength, and natural intelligence of the female body.
Systemic Abuse Disguised as Care
Obstetricians and medicalized midwives have long been portrayed as trusted authorities and guardians of birth, yet beneath this veneer lies a troubling reality. The modern obstetric model is rooted deeply in systemic control, viewing childbirth primarily as a risky, pathological process requiring constant intervention and management rather than a natural physiological event. This approach is not simply misguided but actively harmful, creating a system where care becomes coercion, and support turns into control.
This system thrives financially and structurally by manufacturing crises. Unnecessary interventions like synthetic oxytocin administration, forced membrane sweeps, early inductions, and continuous fetal monitoring are often justified by the notion of ensuring safety, yet these practices frequently create the very emergencies they claim to prevent. Hospitals and care providers benefit directly from higher intervention rates, increased medication use, surgical procedures, and prolonged hospital stays. The financial incentives embedded in this medical framework encourage unnecessary interventions rather than patient-centred, physiological care.
Women frequently experience profound emotional and physical trauma as a direct consequence of these unnecessary interventions. Forced or rushed procedures, painful examinations without proper consent, and coercive language or fearmongering erode women’s autonomy and undermine their self-trust. Birth trauma, postpartum anxiety, depression, and long-term physical health consequences are alarmingly common outcomes of this systemic approach. Babies born within this context suffer terrain imbalances, microbiome disruptions, and neurological disturbances, placing them at increased risk for future physical and emotional health challenges.
Despite abundant evidence exposing the harms of unnecessary medical interventions, hospitals and mainstream obstetricians continue to frame these interventions as essential, life-saving measures. This narrative is perpetuated to justify and normalize abusive practices, dismissing women’s valid concerns and undermining attempts at resistance. Within this system, women’s bodies are treated as defective or inherently problematic, fostering dependency on medical authority rather than self-confidence and bodily autonomy.
Generations of mothers and their babies have endured the lasting damage inflicted by this pervasive medical model. My own grandmother was strapped to a board on her back to give birth, her hands and legs bound! Recognizing these practices as systemic abuse is essential for meaningful change. True care is patient, respectful, empowering, and minimally invasive. It listens, observes, and supports rather than dictates, manipulates, or frightens. Shifting away from medicalized control toward respectful, woman-centred birth practices will restore trust, health, and autonomy, ensuring that childbirth once again becomes a source of strength rather than trauma.
Homebirth and Waterbirth: Restoring Calm and Natural Harmony
Homebirth is the simplest and most powerful way to protect the natural integrity of childbirth. At home, the birthing mother is in her own safe and familiar environment. The privacy of home reduces cortisol and adrenaline, allowing oxytocin to flow naturally. Without the disruptions of hospital protocols, birth unfolds at its own pace, free of stress-induced interruptions. Some women need to eat, be grounded outside, or even sleep and labour will naturally shift or pause if such is needed.
One particularly gentle and powerful method is waterbirth. Birthing in warm water is deeply soothing to tissues and calming but can intensify the birth process which is helpful if stalled. They significantly reduce pain and stress. Warm water relaxes muscles and soft tissues, enabling easier dilation and decreasing the chance of tearing. Water also provides buoyancy, which helps mothers move freely into comfortable positions, empowering us to trust their own bodies.
My training with Waterbirth International (https://waterbirth.org/) during naturopathic college profoundly shaped my understanding of waterbirth’s benefits and I knew if I was called to become a mother, this is how I would birth. The gentle transition from womb to warm water eliminates what is called “air shock,” the jarring experience for the baby moving from warm fluid to cold air. Babies born in water are calm, often opening their eyes underwater, gently moving their limbs, and emerging only when they feel ready. There is no urgency, no forced breathing, just peaceful transition.
Babies born in water are still receiving oxygen through their umbilical cord, so they do not need to breathe immediately upon birth. The reflex that signals readiness to breathe is only activated when the baby’s face touches the air. As a result, there is time and peace, reducing trauma significantly compared to hospital deliveries, which immediately expose the infant to bright lights, cold air, and loud noise.
Lotus Birth: Honouring Natural Transition
One of the most profound ways to support gentle birth is the lotus birth method. A lotus birth allows the umbilical cord and placenta to remain attached to the newborn until the cord naturally separates. The placenta is not medical waste; it is the organ that nourished and grew alongside the baby in utero. Babies form deep connections with their placentas, sometimes cuddling or even kissing them in the womb, as evidenced by ultrasound observations.

My daughter experienced a lotus birth. Her placenta stayed naturally attached to her body for seven days before it gently detached on its own. During this time, we kept the placenta preserved carefully with herbs and salt, wrapped gently, and placed beside her. Allowing the placenta to remain attached until natural separation prevents a traumatic and abrupt severance. It respects the sacredness of birth and provides a calm and gentle transition into the world.
Lotus birth also ensures that the baby receives all of their blood supply, essential nutrients, stem cells, and terrain-supportive substances from the placenta. Immediate cord-cutting deprives babies of these vital resources. Leaving the placenta intact until separation naturally completes the final physiological step of birth, supporting optimal health and vitality in the newborn.
Protecting Natural Birth: Your Sovereign Choice
Choosing homebirth, waterbirth, lotus birth, or a dedicated natural birthing centre (available in some countries) is about reclaiming your sovereignty as a parent and safeguarding your child’s health and well-being from the very first moments of life. By consciously deciding to refuse unnecessary medical interventions, you trust your body’s wisdom, ensuring a peaceful, respectful, and gentle start to your baby’s life.
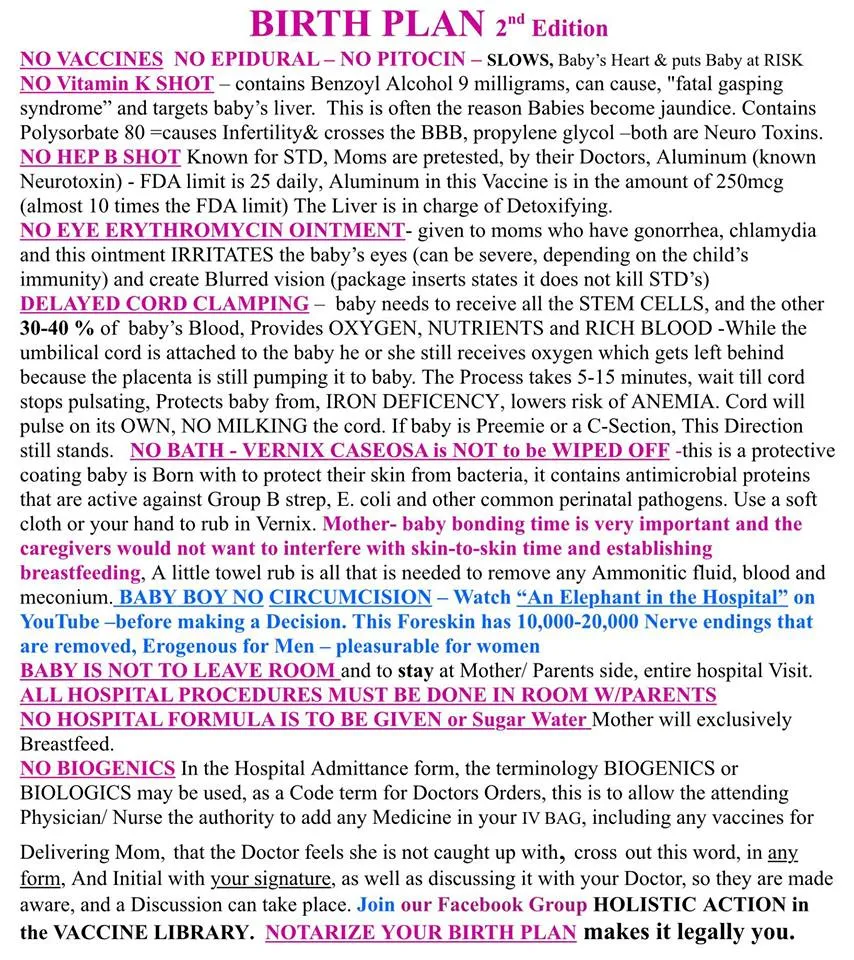
To fully exercise your birth rights, having a clear and comprehensive birth plan prepared in advance is essential. Your birth plan should explicitly state your intentions regarding interventions such as vaccines, vitamin K injections, antibiotics, Pitocin, epidurals, delayed cord clamping, circumcision, bathing, formula feeding, and other routine hospital procedures. A detailed and notarized birth plan acts as a legal document that communicates your explicit wishes, preventing misunderstandings or unauthorized actions from hospital staff.
Identify clearly who will act as the mother’s advocate during labour and birth—ideally, this role will be taken by the father, partner, or a trusted support person who is knowledgeable about your birth plan and can assertively communicate your wishes. The advocate’s role is crucial, as the mother should be fully focused on her birthing process, without being burdened by advocacy or confrontation. The advocate ensures that hospital personnel follow your stated wishes, shielding the birthing mother from unnecessary interruptions, questions, and interference.
Be fully informed about each procedure listed in your birth plan. For example, refusing the routine Vitamin K injection is based on the understanding that the injection contains benzyl alcohol, linked to adverse effects like “fatal gasping syndrome” and liver stress. Similarly, you can refuse the Hepatitis B vaccine, erythromycin eye ointment, and immediate bathing, which removes the protective vernix caseosa crucial to the baby’s initial immune regulation and protection against pathogens. Clarifying your stance against routine hospital practices—such as immediate cord cutting, which prematurely deprives the baby of 30-40% of its crucial blood volume, stem cells, and nutrients—is essential for preserving your baby’s optimal health.
Make it clear that all procedures must be conducted in your presence and that your baby should never be taken away from your sight during the entire hospital stay. Additionally, specify explicitly that you refuse all “biogenics,” “biologics,” or other covert terms hospitals may use to administer drugs without your explicit consent. Awareness of hospital terminology helps prevent the unauthorized administration of drugs or vaccines.
A detailed birth plan and a strong advocate are powerful tools in protecting the birth process from unnecessary medical intervention, safeguarding your sovereignty, and ensuring your baby’s best possible start in life.
Reclaiming Birth as a Natural Process
Birth is not, and never has been, a medical event requiring constant oversight or aggressive management. It is not an emergency, it is an emergence. It is a natural, deeply transformative physiological experience. Childbirth represents the ultimate expression of the body’s wisdom…a profound, regenerative force and a sacred rite of passage that is fully capable of unfolding perfectly without interference and should always be honoured and respected. To reclaim birth is to honour its inherent intelligence, respecting the intricate hormonal dance that orchestrates labour, bonding, and postpartum recovery.
Creating an environment of safety, privacy, and calm allows the body’s innate rhythms to function optimally. Birth thrives on patience, quiet observation, nourishment, emotional connection, and supportive presence. The role of caregivers is not to control or expedite birth but to protect this sacred space, ensuring that unnecessary disruptions and harmful interventions are kept at bay. True support during childbirth is about holding space, trusting the process, and providing gentle encouragement rather than imposing arbitrary timelines or clinical expectations.
To reclaim birth, it is crucial to consciously refuse drugs and interventions unless absolutely necessary. Educating yourself about your rights, clearly communicating your wishes, and asserting bodily autonomy are powerful steps toward protecting yourself and your child from unnecessary medicalization. Seek out caregivers who understand, respect, and encourage physiological birth. Traditional midwives or birth attendants who trust the natural wisdom of the body can offer true guidance, grounded in patience and intuition, not fear and control.
Homebirth and waterbirth offer ideal conditions to support physiological birth. When labour unfolds in familiar, comforting surroundings, free from external pressure, fear diminishes, oxytocin flows naturally, and the birthing process unfolds smoothly. Waterbirth further supports this natural process by providing warmth, buoyancy, comfort, and gentle transition for the newborn, reducing birth stress and trauma. Choosing these gentle methods is a powerful act of reclaiming autonomy, ensuring both mother and child are respected and protected throughout their birth experience.
Birth works flawlessly when we trust and support it rather than control or manipulate it. The medicalized system has proven itself incapable of safeguarding women’s and babies’ well-being, prioritizing profit and convenience over genuine care. To reclaim birth means stepping away from this abusive paradigm and rediscovering the innate wisdom, strength, and intelligence inherent in every birthing body.
Birth does not need fixing. It needs respect. It is time to reclaim this powerful, sacred process, to embrace birth as the profound, natural event it has always been, and to confidently step away from the system that profits from undermining women’s power and trust.
Birth works. The system does not.
References:
- Uvnas-Moberg, K., et al. (2019). The role of oxytocin in stress regulation. Frontiers in Psychology.
- Lederman, Regina P., et al. “The Relationship of Maternal Anxiety, Plasma Catecholamines, and Plasma Cortisol to Progress in Labor.” American Journal of Obstetrics and Gynecology, vol. 132, no. 5, 1978, pp. 495–500.
- Wadhwa, Pathik D., et al. “The Contribution of Maternal Stress to Preterm Birth: Issues and Considerations.” Clinics in Perinatology, vol. 38, no. 3, 2011, pp. 351–384.europepmc.org+1ncbi.nlm.nih.gov+1
- Boulvain, M., et al. (2020). Membrane sweeping for induction of labour. Cochrane Database of Systematic Reviews.
- Buckley, S.J. (2015). Hormonal physiology of childbearing. Childbirth Connection (PDF).
- Simpson, Kathleen Rice, and David C. James. “Effects of Oxytocin-Induced Uterine Hyperstimulation During Labor on Fetal Oxygen Status and Fetal Heart Rate Patterns.” American Journal of Obstetrics and Gynecology, vol. 199, no. 1, 2008, pp. 34.e1-34.e5.
- Zhang, Jun, et al. “Contemporary Patterns of Spontaneous Labor with Normal Neonatal Outcomes.” Obstetrics & Gynecology, vol. 116, no. 6, 2010, pp. 1281–1287.Northwestern Scholars
This study analyzed labor progression in a large cohort of women, providing updated insights into labor patterns and challenging traditional labor curves.ScienceDirect+3ajog.org+3ajog.org+3
- World Health Organization (2015) (aka demons, lol). WHO Statement on Cesarean Section Rates. WHO PDF.
- Keag, Oliver E., et al. “Long-term Risks and Benefits Associated with Cesarean Delivery for Mother, Baby, and Subsequent Pregnancies: Systematic Review and Meta-analysis.” PLOS Medicine, vol. 15, no. 1, 2018, e1002494. PLOS Medicine, doi:10.1371/journal.pmed.1002494.
- Li, Huan, et al. “The Effects of Delivery Mode on the Gut Microbiota and Health: State of Art.” Frontiers in Microbiology, vol. 12, 2021, article 724449.
- Neu, J., & Rushing, J. (2011). Cesarean versus Vaginal Delivery: Long term infant outcomes and the Hygiene Hypothesis. Clinics in Perinatology.
- Moore, E.R., et al. (2012). Early skin-to-skin contact for mothers and babies after birth. Cochrane Database of Systematic Reviews.
- Guise, J.M., et al. (2010). Vaginal birth after cesarean: new insights and evidence. Obstetrics & Gynecology.
- Gaskin, I.M. (2003). Ina May’s Guide to Childbirth. Book on Amazon.
Farm Midwife Website
About Dr. Amandha Dawn Vollmer (ADV)
Dr. Amandha Dawn Vollmer (ADV) is a renowned expert in holistic medicine and a leading authority on the therapeutic use of Dimethyl Sulfoxide (DMSO). With nearly two decades of dedicated research, clinical application, and formulation work, she has become one of the most trusted voices in natural health.
Amandha holds a Bachelor of Science in Agricultural Biotechnology and a Doctorate in Naturopathic Medicine. She is a skilled formulator of natural skincare and handcrafted DMSO-based remedies, creating one-of-a-kind blends that reflect her deep knowledge of terrain health and natural healing.
She is the best-selling author of Healing with DMSO, an accessible and comprehensive guide to using DMSO safely and effectively, complete with practical recipes and protocols. Through her writing, teaching, and speaking, Amandha empowers individuals to take control of their own health, reject medical dogma, and return to the wisdom of nature. Her work continues to inspire and guide thousands toward vibrant, sovereign living.
As a mother of a healthy 13-year-old daughter born at home, into water, with a full lotus birth, no interventions, no vaccines, and no pharmaceuticals, Amandha lives what she teaches. Her daughter has never been to a hospital or medical doctor, only the chiropractor, and is homeschooled. ADV’s life and work are proof that health freedom is not just possible — it is reality for those willing to reclaim it.
Join Amandha’s Private Community!
Participate in specific health related groups, engage with holistic healers, educate yourself with step-by-step online courses, join Amandha in weekly video chats, and reach the ultimate natural health lifestyle.
![]()
Amandha D Vollmer (ADV)
BSc, Herbalist, Reiki Master,
Holistic Health Practitioner,
Degree of Doctor of Naturopathic Medicine
Websites:
Bringing the Wisdom of Nature Education: https://yummy.doctor/
YumNaturals Emporium Store: https://yumnaturals.store/
DMSO Products: https://DMSO.store
Healing with DMSO Book: https://healingwithdmso.com/
Support my Work by Making a Donation:
YUM BTC (Bitcoin) – bc1qayv9rjzlpc8hlc0t5d80le8u0g72f5p75570hz
YUM ETH (Ethereum) – 0xD4AE2Ae316435e4e68DC0c5D2131c2252fD9B0c4
https://yumnaturals.store/product/general-fee-or-donation/
https://www.patreon.com/yumnaturals
Telegram Chats:
1. ADV’s Main Channel: https://t.me/amandhavollmer
2. ADV’s Legal/Lawful Templates Group: https://t.me/HDoT_Templates
3. ADV’s Local Ontario Group: https://t.me/ontarioawake
Advice Disclaimer:
The website content, including but not limited to blogs, newsletters and videos with Amandha Vollmer are intended for general information only, and are not intended to be a substitute for legal, medical or financial advice, and should not be construed as legal, medical or financial advice applicable to your particular situation. No attorney-client or confidential relationship is or will be formed by use of this website or the contents within.

